Canada at risk of missing ambitious target to eliminate disease by 2040 as cervical cancer cases increase
Cervical cancer is now the fastest increasing cancer among females in Canada, putting the country at risk of missing its ambitious target to eliminate the disease by 2040, according to medical and policy experts.
Faltering vaccination rates, barriers to screening and lack of primary care providers are key challenges standing in the way.
“I suspect we’re going to be way behind,” said Karen Yeates, a professor in the department of medicine at Queen’s University who works on improving access to cervical cancer screening in underserved populations. “This is a preventable disease. No woman should die from this.”
A report released in November by the Canadian Cancer Society shows that the incidence of cervical cancer has been rising nearly 4 per cent every year since 2015, the most significant increase in nearly 40 years. The organization estimates that 1,550 people will be diagnosed with the disease in Canada this year. Most cases occur in people under age 50.
“This is quite problematic,” said Samara Perez, assistant professor in the department of oncology at McGill University. “To me, this suggests we’re not moving forward.”
While it’s unclear exactly why the numbers are going up, they have the attention of cancer specialists and policymakers.
“It may just be a little blip, but it’s an increase in those years going up to the pandemic,” said Craig Earle, chief executive officer of the Canadian Partnership Against Cancer. “If we are not to change our approach, that goal of elimination by 2040 could potentially be at risk.”
In 2020, the World Health Organization set a goal of stamping out the disease by 2040, which Canada has agreed to take on by promoting vaccination and improving access to screening and treatment.
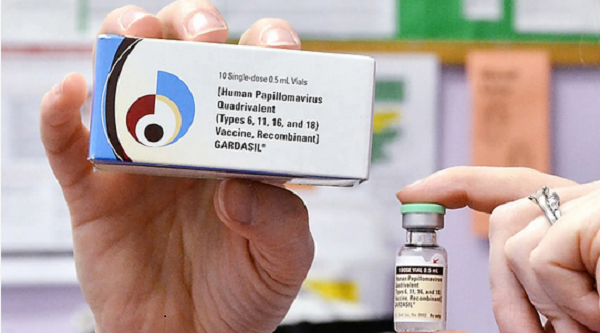
Canada has set three main targets to help reach that goal: by 2025, to have 90 per cent of all 17-year-olds fully vaccinated against human papillomavirus, which causes most cases; by 2030, to have 90 per cent of eligible individuals screened with an HPV test and be up to date with screening; and by 2030, to have 90 per cent of people with abnormal results connected with a clear follow-up plan and to have 90 per cent of those in higher risk groups evaluated using colposcopy, a procedure used to examine the cervix for abnormalities.
A report from the Canadian Partnership Against Cancer published in 2021, based on data from the start of 2020 and earlier, found that only Newfoundland and Labrador had reached the 90 per cent threshold for HPV vaccination coverage for boys and girls. Other provinces and territories reported rates that ranged from 58 per cent to 86 per cent, although several jurisdictions did not report data. (Canada does not have a national vaccine registry.)
Provinces and territories typically administer HPV vaccines in schools, but these programs were upended by pandemic-related disruptions. Two or three doses of HPV vaccines are offered to provide maximum coverage, from Grade 4 to Grade 6 or 7.
Programs across the country offer vaccines to eligible adolescents who missed out on doses, but some data suggest uptake is far below prepandemic levels. For instance, only 23 per cent of all 12-year-olds who missed their HPV vaccination during the 2020-2021 school year were caught up by August, 2022, according to the most recent report from Public Health Ontario.
Screening is also vital, to catch abnormal changes in the cervix that could indicate cancer. Pap tests, in which a health care provider collects cells from the cervix to be analyzed in a lab, have been standard. Canada is slowly moving to adopt HPV tests, which are considered more accurate than Pap smears because they test for the presence of any DNA linked to cancer-causing HPV subtypes.
HPV tests are also more efficient and cost less, as they can be done at home, with samples then sent to a lab by mail. The hope is that this will help boost screening rates, particularly among those who don’t have access to a family doctor or are reluctant to undergo a Pap test. This includes many newcomers who may not previously have had access to any screening and are at heightened risk, Dr. Yeates said.
“We have millions of women in Ontario alone who would fit into the under-screened population,” she said.
Dr. Earle said that while there is hope that widespread availability of HPV tests in the coming years will help prevent cases, one of the challenges is ensuring people who receive an abnormal result are able to easily get follow-up care. Given the shortage of primary care providers, this is not a guarantee and could be a serious problem, he said.
Dr. Perez believes a lack of clear messaging is also part of the problem: HPV vaccination isn’t being discussed often enough or offered to everyone who could benefit. Adults should also be getting vaccinated, for example. It’s possible that stigma is behind some of the reluctance to promote the vaccine more widely, she said, as HPV is transmitted sexually.
“It needs to be framed as a cancer prevention vaccine,” Dr. Perez said.
This article was reported by The Globe and Mail