Top Ontario doctor says COVID, influenza are past peak but urges vigilance
Ontario is past the peak for influenza and RSV activity, and COVID-19 infections are also on a downward trend, welcome signs after the early winter crush of viral illnesses.
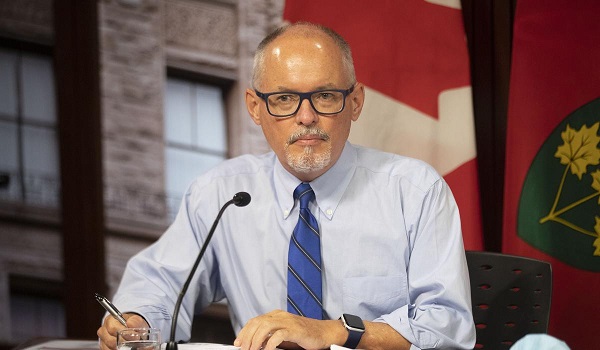
But while the province is “over the worst,” Chief Medical Officer of Health Dr. Kieran Moore warns there is still a long stretch of respiratory season ahead.
“Past the peak doesn’t mean gone from our communities,” Moore told the Star. “We cannot let our guard down.”
Ontario can likely expect four more weeks of influenza A activity, and there is a chance that influenza B will cause another wave of infections later in the season, he said.
And though COVID levels are ticking down, leading to a “reprieve for several months of less activity at a community level,” Moore warned he expects another surge in infections.
“This virus typically cycles in three- to four-month periods, so we’ll be watching in March and April whether new variants are coming forward and what that means to the health of Ontarians.”
Released Thursday, the most recent data from Public Health Ontario shows the provincewide wastewater signal continues to decline. Late last year, the wastewater signal — the most accurate way to determine weekly COVID cases — reached a one-year high.
Dr. Allison McGeer, an infectious disease specialist at Mount Sinai Hospital, said COVID activity remains high in Ontario.
“There’s still a lot of COVID out there,” she said. “We’re still running 30 deaths a week. That’s 1,500 deaths a year in Ontario.”
McGeer, a professor at the University of Toronto’s Dalla Lana School of Public Health, said it’s not yet clear to her that COVID has settled into a regular cycle of three- to four-month waves.
She noted Ontario’s wastewater signal in 2023 “declined steadily from January until sometime in the middle of the summer, and then climbed steadily until December.”
“It’s really hard to know what COVID is planning to do,” she said. “COVID could just keep going at this rate (of infections and hospitalizations) for quite some time.”
McGeer agreed with Moore’s assessment of influenza and RSV activity in the province and said it’s so far been an average season for both viruses.
However, she said the record-number of cases nationwide of invasive Group A strep is “unexpected.” Roughly one in 10 people who get the bacterial infection will die.
In Ontario, there were 222 confirmed cases in December, more than any other month since the 2014-15 season. Between October and December, six children under nine died from the disease.
“When there was a bit of a downturn (in cases) in October, I was hoping that we’d seen the worst of Group A strep,” McGeer said. “But there’s since been a lot of disease — and a lot of severe disease.”
Moore is urging people to stay up to date with their COVID vaccines and says it’s not too late to get a flu shot. He stressed the importance of these vaccines to reduce the risk of getting sick with invasive Group A strep.
“In several cases in Ontario, invasive Group A strep has followed vaccine-preventable diseases like influenza.”
Moore said influenza and RSV peaked in Ontario around the last week of December.
Between Dec. 25 and Jan. 1, there were about 540 people hospitalized with influenza and about 230 people hospitalized with RSV, said Moore, noting that in both cases about 10 per cent of these patients were admitted to intensive care units.
“At the same time, we had significant COVID activity,” he said. “HV. 1 was on the rise and then the JN. 1 subvariant took over and was even more infectious and spread rapidly across Ontario.
“So that ripple effect was significant this year and did have a significant impact on our hospitals at a difficult time.”
Heading into February, Moore said the hospital system is in a “much better position.” As of Jan. 29, there were 324 people in hospital with influenza, 121 with RSV and 945 with COVID, he said. At the peak of the current COVID wave, there were about 1,700 people with the virus in hospital, he said.
Moore said hospitals typically pause scheduled surgeries between Dec. 23 and Jan. 2 but since then “surgical care has continued on uninterrupted.” In previous years, hospitals were forced to cancel scheduled surgeries to care for patients with viral illnesses.
Moore said about 46 per cent of people 65 and older have received the updated COVID vaccine that targets XBB variants. In long-term-care facilities, 68 per cent of residents have gotten the updated shot, while 63 per cent of residents in retirement homes have gotten the new vaccine.
About 15 per cent of the general population have received the XBB shot, he said, noting Ontario’s COVID vaccine coverage is comparable to other provinces, but lower than some countries, such as the United Kingdom, which vaccinated 60 to 70 per cent of its older population.
While there isn’t yet a detailed picture on the number of Ontarians who got a flu shot this season, Moore said it’s clear there has been a “much higher uptake of influenza vaccine than COVID vaccine.”
“We were recommending getting both at the same time, especially if you’re vulnerable,” he said. “Somehow that message, people didn’t take up. So we’ll have to review our communication strategy for next year and our recommendations for next year.”
McGeer agreed that it’s important to understand why there is a gap in uptake between the COVID and influenza vaccines. She said in an average influenza year, Ontario records a little over 1,000 flu deaths. Public Health Ontario data shows that in 2023, more than 1,500 people died of COVID.
“You would think anybody who’s getting their flu vaccine would be somebody who’s getting a COVID vaccine. But it’s clearly not how people are feeling and that’s something we need to understand.”
This article was reported by The Star